The mission of physics research is to develop new techniques and investigate new methodologies to continuously improve treatment planning and evaluation methods; target localization and verification accuracy; and refine treatment delivery precision.
Our physics faculty investigators are actively engaged in research in the following domains of radiation therapy physics.
|
Research Domain |
Core Focus |
Investigators |
|---|---|---|
|
AI-Driven RT |
Automation, prediction, adaptation |
Jackie Wu, Qiuwen Wu, Sheng Yang, Deshan Yang, Chunhao Wang, Kyle Lafata, Yunfeng Cui, Ke Lu |
|
FLASH and UHDR |
Radiobiology, dosimetry |
Mark Oldham |
|
Functionally and Biologically Guided RT |
Functional & genomic adaptation |
Chunhao Wang, Kyle Lafata, Mark Oldham, Yunfeng Cui, Deshan Yang |
|
Image-Guided Adaptive RT |
Real-time, MRI/PET-based targeting, motion management |
Deshan Yang, Chunhao Wang, John Ginn, Yunfeng Cui, Tyler Hornsby, Ke Lu, Jackie Wu, Sheng Yang |
|
Particle Therapy |
Proton/carbon/VHEE physics |
|
|
QA |
Patient, device, and plan-specific QA |
Justus Adamson, Sua Yoo, Mark Oldham, Jennifer O’Daniel, Will Giles, Guoqiang Cui |
|
Radiomics and Big Data |
Imaging biomarkers, outcome prediction |
Kyle Lafata, Chunhao Wang |
|
Radiobiology |
RT-immunotherapy synergy |
Kyle Lafata, Casey Lee, Mark Oldham |
|
Automation |
Real-time control, precision delivery, treatment planning |
Justus Adamson, Yunfeng Cui, Deshan Yang, Jackie Wu, Sheng Yang |
|
Theranostics |
Imaging, AI, RT physics, dosimetry, automation |
Deshan Yang, Kyle Lafata, Mark Oldham |
Click the plus signs below for an in-depth overview of each research domain's projects.
AI-Driven RT
Research Overview
In traditional practice, IMRT/VMAT planning takes an experienced planner 1-6 hours, using an iterative, trial-and-error approach. Even with this effort, the search for patient-specific optimal organ sparing is still strongly influenced by the planner’s experience. Significant variations in plan quality have been observed at different institutions. Experienced centers are generally more capable of maximizing the dosimetric advantages of IMRT/VMAT. The knowledge and experience of an IMRT/VMAT treatment team is of great importance to realize the full benefits of this advanced technology.
Our research focuses on areas of treatment planning, automation, optimization and AI applications. Specifically, we focus on developing knowledge models and AI models for guiding IMRT/VMAT planning. The models are carefully developed from databases of high-quality clinical plans and guidelines from clinical studies, as well as personal experience of expert planners. This comprehensive modeling approach with a strong focus on clinical practice is a distinguishing feature of this technology. These advanced AI models will:
- Capture human expert knowledge in designing high-quality plans
- Predict the optimal organ sparing that is specific to an individual patient, and
- Guide the design of the treatment plan to achieve optimal dose distribution with improved efficiency.
By capturing clinical experience of the entire planning process, including various trade-off decisions, into an integrated ecosystem of multiple AI models, we hope to accomplish a complete AI planning workflow that allows robust plan quality and flexible plan customization based on the physician’s preferences and the patient’s anatomy.
Investigators
Funding Sources
Varian Medical System
Selected Publications
- Li T, Zhu X, Thongphiew D, Lee WR, Vujaskovic Z, Wu Q, Yin FF, and Wu QJ. On-line Adaptive Radiation Therapy (ART): Feasibility And Clinical Study, J Oncol., vol. 2011
- Li T, Thongphiew D, Zhu X, Lee WR, Vujaskovic Z, Yin FF, and Wu QJ. Adaptive prostate IGRT combining online re-optimization and re-positioning: a feasibility study. Phys. Med. Biol. 56: 1243, 2011
- Yuan L, Ge Y, Lee WR, Yin FF, Kirkpatrick JP, Wu QJ. Quantitative analysis of the factors which affect the interpatient organ-at-risk dose sparing variation in IMRT plans. Med Phys. 2012 Nov; 39(11):6868-78.
- Yuan L, Wu QJ, Yin F, Li Y, Sheng Y, Kelsey CR, Ge Y. Standardized beam bouquets for lung imrt planning. Physics in medicine and biology 2015;60:1831-1843.
- Sheng Y, Li T, Zhang Y, Lee WR, Yin FF, Ge Y, Wu QJ: Atlas-guided prostate intensity modulated radiation therapy (IMRT) planning. Phys Med Biol 2015, 60:7277-7291.
- Zhang J, Wu QJ, Xie T, Sheng Y, Yin FF, Ge Y. An Ensemble Approach to Knowledge-Based Intensity-Modulated Radiation Therapy Planning. Front Oncol. 2018 Mar 19;8:57.
- Sheng Y, Li T, Yoo S, Yin F-F, Blitzblau R, Horton JK, Ge Y, Wu QJ. Automatic Planning of Whole Breast Radiation Therapy Using Machine Learning Models. Frontiers in Oncology. 2019 Aug 7;9:1-8.
- Zhang J, Ge Y, Sheng Y, Wang C, Zhang J, Wu Y, Wu Q, Yin FF, Wu QJ, Knowledge-based Tradeoff Hyperplanes for Head-and-neck Treatment Planning. Int J Radiat Oncol Biol Phys. 2020;106(5):1095-1103.
- Wang W, Sheng Y, Wang C, Zhang J, Li X, Palta M, Czito B, Willett C, Wu Q, Ge Y, Yin FF, Wu QJ, Fluence Map Prediction Using Deep Learning Models-Direct Plan Generation for Pancreas Stereotactic Body Radiation Therapy. Frontiers in Artificial Intelligence. 2020;3:68.
- Mistro M, Sheng Y, Ge Y, Kelsey K, Palta J, Cai J, Wu Q, Yin FF, Wu QJ, Knowledge Models as Teaching Aid for Training Intensity Modulated Radiation Therapy Planning: A Lung Cancer Case Study . Frontiers in Artificial Intelligence. 2020;3:66.
- Li X, Zhang J, Sheng Y, Chang Y, Yin FF, Ge Y, Wu QJ, Wang C, Automatic IMRT Planning via Static Field Fluence Prediction (AIP-SFFP): A Deep Learning Algorithm for Real-time Prostate Treatment Planning . Phys Med Biol. 2020;10.1088/1361-6560/aba5eb.
- Zhang J, Wang C, Sheng Y, Palta M, Czito B, Willett C, Zhang J, Jensen P, Yin FF, Wu Q, Ge Y, Wu QJ, An Interpretable Planning Bot for Pancreas Stereotactic Body Radiation Therapy. Int J Radiat Oncol Biol Phys. 2021;109:1076-1085.
- Li X, Wang C, Sheng Y, Zhang J, Wang W, Yin FF, Wu Q, Wu QJ, Ge Y. An artificial intelligence-driven agent for real-time head-and-neck IMRT plan generation using conditional generative adversarial network (cGAN). Med Phys 2021;48:2714-23.
- Li X, Ge Y, Wu Q, Wang C, Sheng Y, Wang W, Stephens H, Yin F-F, Wu QJ. Input feature design and its impact on the performance of deep learning models for predicting fluence maps in intensity-modulated radiation therapy. Physics in Medicine & Biology 2022;67:215009.
Research Overview
While AI algorithms, particularly deep learning applications, are increasingly outperforming humans in various diagnostic and predictive tasks in medicine, their clinical deployment remains challenging. One key factor is the 'black box' nature of current AI systems in health care, meaning their internal mechanics and decision-making processes cannot be easily understood by practitioners using existing medical domain knowledge and long-term clinical experience. This issue leads to a lack of accountability and trust in AI applications in clinical settings. My research focuses on developing novel AI algorithms that incorporate explainability from current human knowledge, including biological models, genetic profiling, computational image biomarkers and pathology screening. I utilize advanced mathematical tools to investigate new deep learning structures with explainability. The objective of this series of work is to establish a framework for building task-specific AI models based on our multidisciplinary background in radiation oncology, mathematics and computer science. Ultimately, this research aims to promote AI applications in radiation oncology clinics with human confidence, by creating algorithms that are both effective and easily understandable by health care professionals.
This body of work is supported by NIH P30 institutional support CA014236.
Investigator
Selected Publications
- Zhao J, Vaios E, Yang Z, Lu K, Floyd S, Yang D, Ji H, Reitman Z, Lafata K, Fecci P, Kirkpatrick J, Wang C*. Radiogenomic Explainable AI with Neural Ordinary Differential Equation for Identifying Post-SRS Brain Metastasis Radionecrosis. Medical Physics 52(4)(2025): 2661-2674
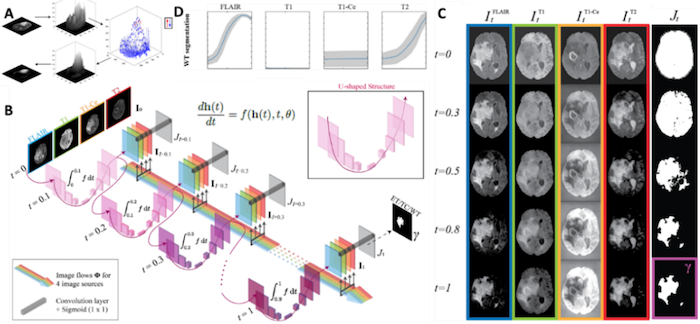
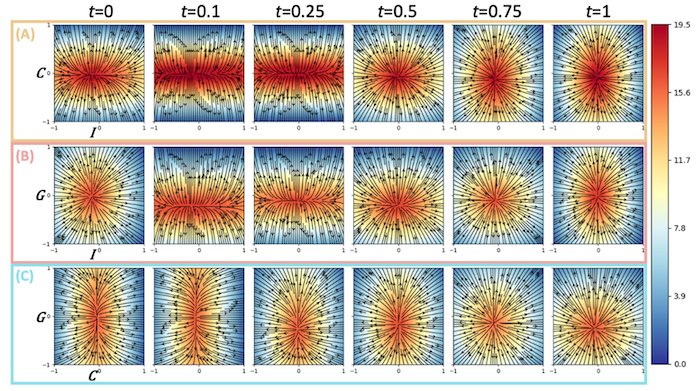
- Yang Z, Hu Z, Ji H, Lafata K, Floyd S, Yin F-F, Wang C*. A Neural Ordinary Differential Equation Model for Visualizing Deep Neural Network Behaviors in Multi-Parametric MRI based Glioma Segmentation. Medical Physics 50 (8) (2023): 4825 (2023 Editor’s Choice Research Article)
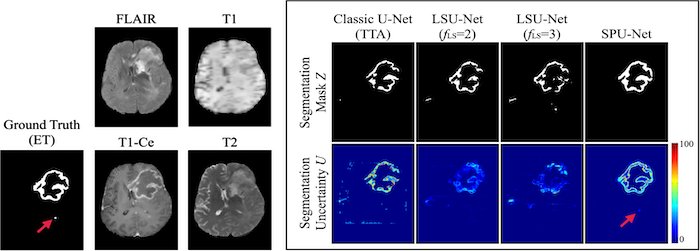
- Chen Y, Yang Z, Zhao J, Adamson J, Sheng Y, Yin F-F, Wang C*. A radiomics-incorporated deep ensemble learning model for multi-parametric MRI-based glioma segmentation. Physics in Medicine and Biology 68 (18) (2023): 185025
- Ji H, Lafata K, Mowery Y, Brizel D, Bertozzi A, Yin F-F, Wang C*. Post-Radiotherapy PET Image Outcome Prediction by Deep Learning under Biological Model Guidance: A Feasibility Study of Oropharyngeal Cancer Application. Frontiers in Oncology 12 (2022): 895544
- Wang C*, Liu C, Lafata K, Chang Y, Cui Y, Li X, Mowery Y, Brizel D, Yin F-F. Dose-Distribution-Driven PET Image-based Outcome Prediction (DDD-PIOP): A Framework Design for Oropharyngeal Cancer IMRT Application. Frontiers in Oncology 10 (2020): 1592.
Research Overview
Our research focuses on segmentation of cardiac substructures using a deep-learning method. This study aims to develop an auto-segmentation method for various heart substructures to aid radiotherapy treatment planning.

Investigators
Research Overview
Real-time motion tracking of abdominal tumors, including LAPC, on regular x-ray LINAC machines is an unsolved problem in radiation therapy. We are developing novel imaging methods and AI models to continuously and accurately monitor and track the 3-dimensional respiratory motion of the tumor targets and organs-at-risk on the radiation treatment day. The novel solutions will allow for precisely directing the radiation beams to the moving tumor, reducing gastrointestinal radiation toxicity and increasing the treatment effectiveness and overall survival.
Read more about real-time motion tracking and motion management research.
Investigators
Research Overview
A 4D convolutional neural network model was developed to reduce the streak artifacts induced by sparse and clustered phase binning. The 4D gated-FDK images served as the input, and the outputs were the artifact-removed images. A lightweight separable 4D convolution module was designed to process all phase-gated 4D CBCT images as a whole 4D volume and fully utilize the correlated image information among all 4D phases.
Investigators
Research Overview
It is critical to precisely define the critical cardiac substructures regardless of the motion in the CT images, and to accurately assess both respiratory and cardiac motion of these critical substructures. The regularly used respiratory 4DCTs ignore cardiac motion from the respiratory phase rebinning step, and thus have severe cardiac motion artifacts and cannot accurately inform either cardiac motion or respiratory motion of the heart. Breath-hold cardiac 4DCTs are useful for assessing cardiac-only motion and defining cardiac substructures in the breath-hold state of image acquisition. Because cardiac motion and respiratory motion are not entirely independent, it is ineffective and inadequate to assess the respiratory and cardiac motion of the heart separately on the r4DCTs and c4DCTs. It is necessary to develop a new 5DCT imaging protocol to image patients breathing freely and relaxedly, thus to capture both respiratory motion and cardiac motion simultaneously.
Investigators
FLASH and UHDR
Research Overview
Our research investigates the efficacy of FLASH radiation therapy, where radiation is delivered to tumors at vastly higher dose-rates than in conventional therapy. FLASH is a new therapeutic paradigm that has generated tremendous interest and excitement because side effects, like normal tissue damage, are greatly reduced, while the efficacy of tumor treatment is preserved.
For challenging diseases like brain cancer, FLASH offers the potential for more effective treatments, and even complete remission. We are fortunate to have access on the Duke campus to one of the few research LINACs in the world that can generate dose rates in excess of 20MGy/s, enabling unique mechanistic explorations of FLASH here at Duke. This project is part of a funded collaboration (Duke Cancer Center Research Grant) with co-PIs Dr. Scott Floyd (MD, Radiation Oncologist) and Professor Ying Wu (Physics Department). There is also scope for simulating the FLASH treatments and effects using the Monte Carlo TOPAS tool, and the nBio extension.
Investigators
Adaptive RT, Functional and Biological Guidance
Research Overview
This research utilizes the unique and complementary information that functional PET imaging provides to assist in clinical tasks in radiation therapy, including target delineation, treatment adaptation, treatment response prediction and more.

Investigators
Selected Publications
- Hong JC, Cui Y, Patel BN, Rushing CN, Faught A, Eng J, Higgins K, Yin FF, Das SK, Czito B, Willett CG, Palta M. Association of interim FDG-PET imaging during chemoradiation for squamous anal canal carcinoma with recurrence. International Journal of Radiation Oncology * Biology * Physics 2018; 102(4):1046-1051.
- Tandberg DJ, Cui Y, Rushing CN, Hong JC, Ackerson BG, Marin D, Zhang X, Czito BG, Willett CW, Palta M. Intra-treatment response assessment with 18F-FDG PET: Correlation of semi-quantitative PET features with pathologic response of esophageal cancer to neoadjuvant chemoradiotherapy. International Journal of Radiation Oncology * Biology * Physics 2018; 102(4): 1002-1007.
- Cui Y, Bowsher J, Cai J, Yin FF. Impact of moving target on measurement accuracy in 3D and 4D PET imaging—a phantom study. Advances in Radiation Oncology 2017; 2(1): 94-100.
- Zhao F, Cui Y, Li M, Fu Z, Chen Z, Kong L, Yang G, Yu J. Prognostic value of 3’-Deoxy-3’-18F- Fluorothymidine ([18F] FLT PET) in patients with recurrent malignant gliomas. Nuclear Medicine and Biology 2014; 41(8): 710-715.
Research Overview
Computed tomography (CT) is the primary imaging modality in modern radiotherapy, offering unique tissue electron density information for accurate dose calculation. Over the last decade, the application of magnetic resonance imaging (MRI) in radiotherapy has emerged as a significant research topic. MRI offers superior soft tissue contrast for disease identification, zero risk of ionizing radiation and the potential to provide physiological information in addition to anatomical details. This body of work advances MRI applications in various aspects of radiotherapy, including four-dimensional (4D) MRI for tumor motion assessment, rapid MR image reconstruction and MRI-specific image biomarkers for radiotherapy. Some of these findings have been incorporated into medical physics practice guidelines within our community.
This body of work is supported by NIH P30 institutional support CA014236 and NIH/NCI R01CA289261.
Investigator
Selected Publications
- Zhao J, Vaios E, Wang Y, Yang Z, Cui Y, Reitman ZJ, Lafata KJ, Fecci P, Kirkpatrick J, Fang Yin F, Floyd S, Wang C*. Dose-Incorporated Deep Ensemble Learning for Improving Brain Metastasis Stereotactic Radiosurgery Outcome Prediction. International Journal of Radiation Oncology* Biology* Physics 120(2): 603-613 (2024)
- Yang Z, Lafata K, Vaios E, Hu Z, Mullikin T, Yin F-F, Wang C*. Quantifying U-Net Uncertainty in Multi-Parametric MRI-based Glioma Segmentation by Spherical Image Projection. Medical Physics 51(3) (2024): 1931-1943
- Wang C*, Yin F-F. 4D-MRI in Radiotherapy. In: Magnetic Resonance Imaging, ISBN 978-1-78923-822-8. London, UK: IntechOpen (2019)
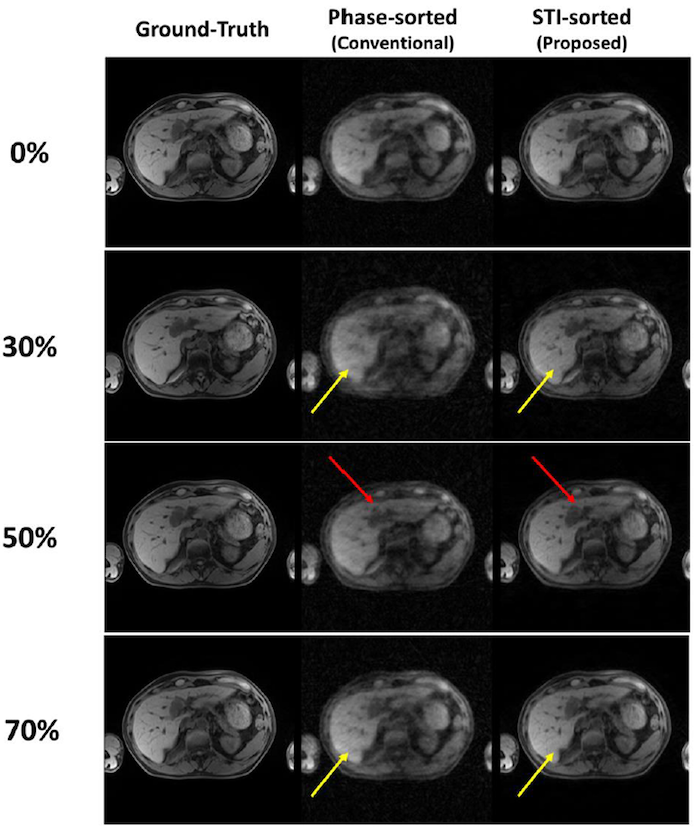
- Wang C*, Subashi E, Yin F-F, Chang Z, Cai J. A Spatiotemporal-Constrained Sorting Method for Motion-robust 4D-MRI: A Feasibility Study. International Journal of Radiation Oncology* Biology* Physics 103(3): 758-766 (2019)
- Wang C*, Subashi E, Liang X, Yin F-F, Chang Z. Evaluation of the Effect of Transcytolemmal Water Exchange Analysis for Therapeutic Response Assessment using DCE-MRI: A Comparison Study. Physics in Medicine and Biology 67 (13) (2017): 4763-4780
Research Overview
- 3D motion modeling
- Accelerate motion assessment
- Enable real-time 3D motion evaluation from 2D cine imaging
- Motion prediction
- Overcome radiation gating latencies
- Enable target MLC-tracking

Investigators
Research Overview
- Improve image quality by reducing motion artifacts
- Enable robust treatment planning in the presence of motion to ensure effective treatment

Investigators
Research Overview
This study is aiming to develop advanced dynamic conformal arc (DCA) planning techniques, by iteratively adjusting the MLC aperture shape of each control points based on intermediate dose calculation, to improve lung SBRT planning quality.
Investigators
Selected Publication
- Erickson B, Ackerson B, Kelsey C, Yin F, Adamson J, Cui Y. The effect of various dose normalization strategies when implementing linear Boltzmann transport equation dose calculation for lung SBRT planning. Practical Radiation Oncology 2022; 12(5): 446-456
Research Overview
IGRT has been widely applied in radiation therapy to use various imaging tools to improve the localization accuracy of the treatment. With the development of flat panel detectors, cone-beam CT (CBCT) has become a key imaging tool in IGRT, which is able to provide volumetric information about the patient for 3D or 4D target localization. MRI is another valuable tool under intensive study which is useful for target delineation and treatment assessment. Our group’s focus is to develop novel image acquisition and reconstruction techniques to improve the image quality and reduce imaging dose for various imaging modalities in IGRT.
Specifically, we are focusing on the following directions:
- Imaging dose reduction using digital tomosynthesis (DTS). DTS only uses limited angle projections to reconstruct quasi-3D images; therefore it has much lower imaging dose than CBCT. This project is to evaluate the efficacy of DTS image guidance for different anatomic sites, including head-and-neck, prostate, breast, liver and lung.
- Development of clinical platform for DTS application. This project focuses on accelerating reconstruction using graphics card and developing user-friendly GUI interface for clinical use.
- Image reconstruction using prior knowledge and deformation models. A new method is developed to reconstruct full 3D images from limited-angle projections using patient prior knowledge and deformation models. Different deformation models, including PCA based motion models (MM) and free-form deformation (FD) model, are explored to improve the accuracy and efficiency.
- CBCT scatter correction. A synchronized moving grid (SMOG) system is being developed to correct for scatter, image lag and gantry flex of the flat panel detector based cone-beam CT (CBCT) system.
- Dual source CBCT. A dual source CBCT system has been built and its performance is being characterized. Virtual monochromatic (VM) and linearly mixed (LM) CBCTs are also developed to investigate their potential applications in metal artifact reduction and contrast enhancement in IGRT.
- Marker-less self-sorted 4D-CBCT. To develop an automatic projection sorting algorithm based on Fourier transformation of the projections.
- Fast reconstruction and processing of MR water-fat imaging, angiography and quantitative functional imaging such as diffusion and perfusion imaging along with its clinical applications.
Investigators
Funding Sources
- NIH-NCI
- Varian Medical System
Selected Publications
- D. J. Godfrey, F. F. Yin, M. Oldham, S. Yoo, C. Willett, “Digital tomosynthesis using an on-board kV imaging device,” Int. J. Radiat. Oncol. Biol. Phys. 65(1), 8-15 (2006).
- Q. J. Wu, D. J. Godfrey, Z. Wang, J. Zhang, S. Zhou, S. You, D. Brizel, F. Yin, ”On-board patient positioning for head and neck IMRT: comparing digital tomosynthesis to kV radiography and cone-beam CT.” Int. J. Radiat. Oncol. Biol. Phys. 69(2), 598-606 (2007).
- D. J. Godfrey, L. Ren, H. Yan, Q. Wu, S. Yoo, M. Oldham, F. Yin, “Evaluation of three types of reference image data for external beam radiotherapy target localization using digital tomosynthesis (DTS).” Med. Phys. 34(8) 3374-3384 (2007).
- H. Yan, L. Ren, D. J. Godfrey, F. Yin, “Accelerating reconstruction of reference digital tomosynthesis using graphics hardware.” Med. Phys. 34(10), 3768-3776 (2007).
- L. Ren, D. J. Godfrey, H. Yan, Q. J. Wu, F. Yin, “Automatic registration between reference and on-board digital tomosynthesis images for positioning verification.” Med. Phys. 35, 664 (2008).
- H. Yan, D. J. Godfrey, F. Yin, “Fast reconstruction of digital tomosynthesis using on-board images.” Med. Phys. 35, 2162 (2008).
- L. Ren, J. Zhang, D. Thongphiew, D. J. Godfrey, Z. Wang, F. Yin, “A novel digital tomosynthesis (DTS) reconstruction method using a deformation field map.” Med. Phys. 35, 3110 (2008).
- J. Maurer, D. J. Godfrey, Z. Wang, F. Yin, “On-board four-dimensional digital tomosynthesis: First experimental results.” Med. Phys. 35, 3574 (2008).
- S. Yoo, Q. J. Wu, D. J. Godfrey, H. Yan, L. Ren, S. Das, W. R. Lee, F. Yin, “Clinical evaluation of positioning verification using digital tomosynthesis (DTS) based on bony anatomy and soft tissues for prostate image-guided radiation therapy (IGRT).” Int. J. Radiat. Oncol. Biol. Phys. 73(1):296-305 (2009).
- J. Zhang, Q. J. Wu, D. J. Godfrey, T. Fatunase, L. B. Marks, F. Yin, “Comparing digital tomosynthesis to cone-beam CT for position verification in patients undergoing partial breast irradiation,” Int. J. Radiat. Oncol. Biol. Phys. 73(3):952-957 (2009).
- Z. Chang, Q. Xiang, J. Ji, and F.F. Yin, “Efficient Multiple Acquisitions by Skipped Phase Encoding and Edge Deghosting (SPEED) Using Shared Spatial Information,” Magn. Reson. Med. 61:229–233 (2009).
- Z. Chang, Q. Xiang, H. Shen, and F.F. Yin, “Accelerating Non-Contrast-Enhanced MR Angiography with Inflow Inversion Recovery Imaging by Skipped Phase Encoding and Edge Deghosting (SPEED),” Journal of Magnetic Resonance Imaging 31:757-765 (2010).
- J Maurer, T Pan, F Yin, “Slow gantry rotation acquisition technique for on-board four-dimensional tomosynthesis.” Med Phys 37:921-933 (2010).
- J. Jin, L. Ren, Q. Liu, J. Kim, N. Wen, H. Guan, B. Movsas, I. Chetty, “Combining scatter reduction and correction to improve image quality in cone-beam computed tomography (CBCT)”, Med. Phys. 37, 5634-5644, (2010).
- Q. J. Wu, J. Meyer, J. Fuller, D. Godfrey, Z. Wang, J. Zhang, F. Yin, “Digital tomosynthesis for respiratory gated liver treatment: Clinical feasibility for daily image guidance,” Int. J. Radiat. Oncol. Biol. Phys.79(1):289-296 (2011).
- I. Vergalasova, J. Cai, F.F. Yin, “A novel technique for markerless, self-sorted 4D CBCT: feasibility study,” Med Phys 39(3):1442-1451 (2012).
- L. Ren, I. Chetty, J. Zhang, J. Jin, Q.J. Wu, H. Yan, D.M. Brizel, W.R. Lee, B. Movsas, F. Yin, “Development and clinical evaluation of a three-dimensional cone-beam computed tomography estimation method using a deformation field map,” Int J Radiat Oncol Biol Phys, 82(5): 1584-93 (2012).
- L. Ren, F. Yin, I. Chetty, D. Jaffray, and J. Jin, “Feasibility study of a synchronized-moving-grid (SMOG) system to improve image quality in Cone-Beam Computed Tomography (CBCT)”, Med. Phys., 39(8), 5099-5110, (2012).
- H. Li, W. Giles, L. Ren, J. Bowsher and F.F. Yin, “Implementation of Dual-Energy Technique for Virtual Monochromatic and Linearly Mixed CBCTs”, Med. Phys. 39(10), 6056-64, 2012.
- Z. Chang, Q. Xiang, H. Shen, J. Ji and F.F. Yin, "Accelerating Phase Contrast MR Angiography by Simplified Skipped Phase Encoding and Edge Deghosting with Array Coil Enhancement,” Med. Phys., 39:1247-1252 (2012).
- H. Li, W. Giles, J. Bowsher and F.F. Yin, “A Dual Cone-Beam CT System for Image Guided Radiotherapy: Initial Performance Characterization”, Med. Phys. 40(2), 021912, 2013z
Research Overview
It is critical to quantitatively assess the cardiac motion and respiratory motion of the heart to determine the motion margin for treatment planning and optimization. We developed novel image processing methods to compute heart motion in the breath-hold cardiac 4DCTs and the free-breathing respiratory 4DCTs.
Read more about stereotactic arrhythmia radioablation and cardiac motion management research.
Investigators
Dosimetry and QA
Research Overview
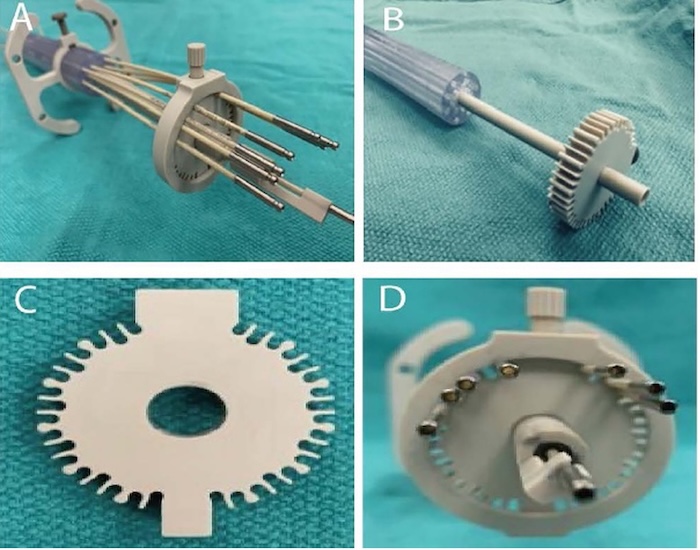
3D printing technology has been widely used in radiation therapy. In brachytherapy, we will manufacture patient-specific brachytherapy applicators (see figures below, both from other institutions) for gynecological cancer treatment and eye plaque brachytherapy, development of new brachytherapy QA phantoms as well as clinically relevant devices to improve brachytherapy procedures.
Investigators
Research Overview
The lab pursues two main avenues of research.
The first involves developing and applying new methods of high-resolution 3D dosimetry. A range of uniquely capable state-of-the-art 3D dosimetry systems has been developed with funding support from the National Institute of Health. These systems are currently being applied to a diverse range of challenges in both the clinical (radiation therapy) and research domains.
The second direction focuses on developing the new optical bio-imaging techniques of optical-computed-tomography (optical-CT), and optical-emission-computed-tomography (optical-ECT). These techniques have the potential to provide uniquely useful information on biological processes in bulk tumor and tissue samples.
Read more about 3D dosimetry and optical bio-imaging research.
Investigator
Research Overview
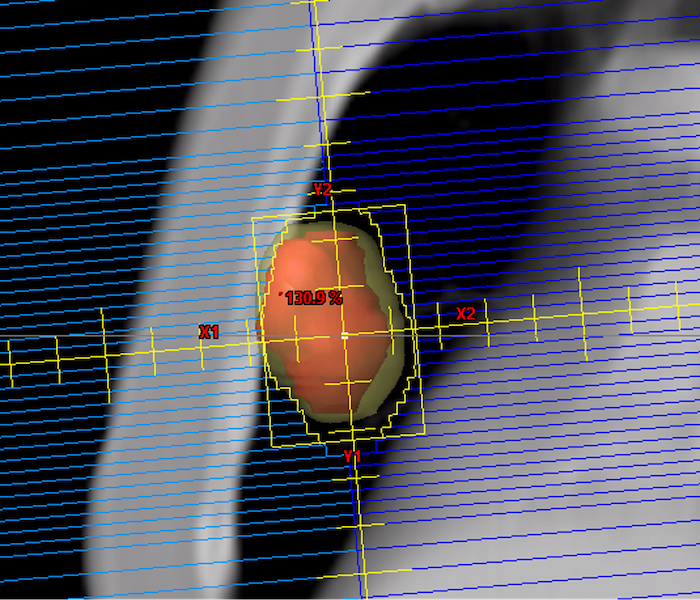
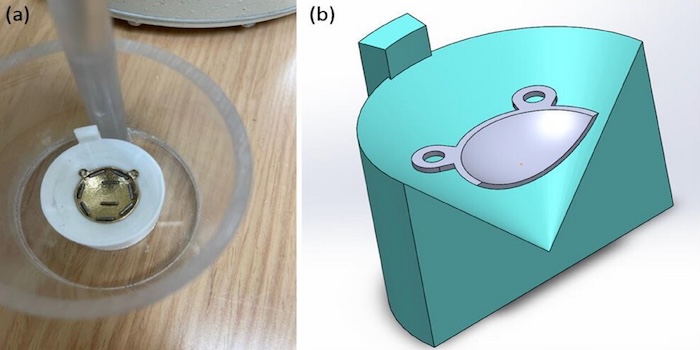
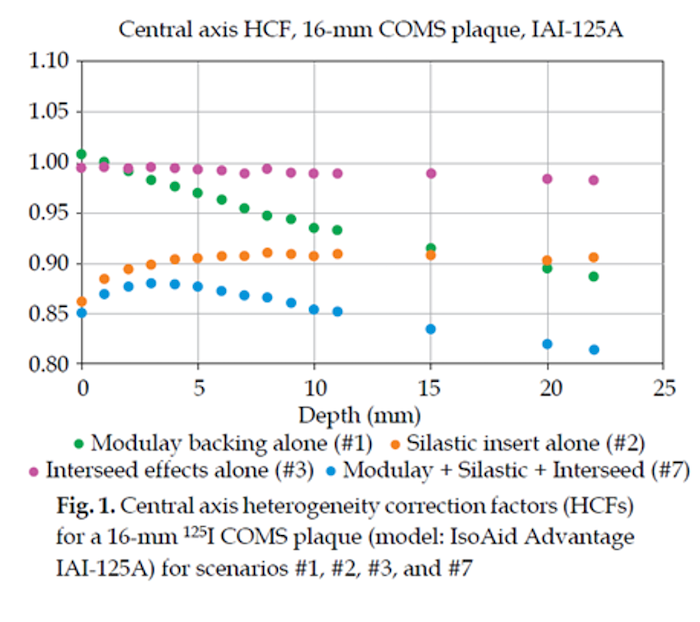
Our research focuses on investigating the model-based dose calculation in eye plaque brachytherapy and HDR brachytherapy. We reported heterogeneity dose correction factors (see two figures below) for COMS eye plaque brachytherapy using egs-brachy code.

Investigator
Selected Publication
- Lee YC, Akhtar MN, Kim Y, Jung JW. Sensitivity of contributing factors to heterogeneity corrections in dosimetry of ocular brachytherapy using iodine-125 COMS plaques. J Contemp Brachytherapy. 2024 Oct;16(5):371-382. doi: 10.5114/jcb.2024.144232. Epub 2024 Oct 18. PMID: 39719954; PMCID: PMC11664798.
Research Overview
Prospective Risk Assessment for Quality Assurance Devices
When performing QA measurements, the limitations of the QA device must be well understood. AAPM's TG-360 is developing recommendations to characterize these devices. Our research involves an international prospective risk assessment to determine which errors are the most relevant to test for these devices.
Prospective Risk Assessment for Plan-Specific Quality Assurance
It is important to consider the clinical process as a whole when making changes to quality assurance technologies. How do the quality assurance (QA) interventions work together to ensure that the relevant failures are caught prior to patient treatment? We propose a novel structured method using failure modes and effects analysis (FMEA) to assess combinations of QA technologies rather than as stand-alone tools, and we apply this specifically for the IMRT Patient Specific QA (PSQA) process. This technique may be used to assess how new QA tools fit into an existing workflow, either based on all potential failure modes, on those with the highest severity, or on those with the highest risk-priority score. As not all clinics have the time, resources and/or expertise to perform a full FMEA, we hope this work can provide some of the benefits of an FMEA to those sites.
Plan-Specific Quality Assurance: Simulation vs. Measurement
In radiation oncology, radiation treatments utilizing intensity modulation (IMRT) have a recognized higher risk of delivery error than simpler 3D plans. Intensity modulation involves multiple moving components, dose rate variation versus static components and dose rate for 3D. These potential errors come from three sources: insufficient radiation beam models in the treatment planning systems, data transfer errors between treatment planning and treatment delivery computers and hardware/software errors of the linear accelerator, particularly the multi-leaf collimator (MLC). To validate each IMRT plan prior to its treatment, we have traditionally performed a quality assurance measurement with a physical device. Doubts have been raised regarding whether a measurement-based approach is sufficiently effective at detecting errors. It has been shown that 2D QA measurements could not accurately separate failing and passing plans. Even when the AAPM’s TG-119 procedures for IMRT validation are followed, large local dose differences can still be present. A large comparison of six common QA devices showed that “all of the evaluated devices performed poorly at identifying unacceptable plans." As a result, research is ongoing into methods to improve the sensitivity of our IMRT QA. A calculation-based approach has been shown to be more effective than a measurement-based approach in predicting plan acceptability. AAPM TG-219 suggested switching to a hybrid measurement/calculation approach, if the independent calculation is done with highly accurate 3D algorithms as opposed to the less sensitive 1D algorithms. An AI-based approach to predicting MLC positional discrepancies also has potential. This research protocol investigates whether a new simulation-based approach is equivalent to or improves upon the standard measurement-based approach.
Investigators
Funding Sources
Scandidos, Inc.
Selected Publications
- O’Daniel JC, Giles W, Cui Y, Adamson J. A structured FMEA approach to optimizing combinations of plan-specific quality assurance techniques for IMRT and VMAT QA. Med Phys, epub 2023. https://doi.org/10.1002/mp.16630
- O’Daniel JC, Giles W, Cui Y, Adamson J. A structured FMEA approach to optimizing combinations of plan-specific quality assurance techniques for IMRT and VMAT QA. Med Phys, epub 2023. https://doi.org/10.1002/mp.16630.
- Lay LM, Chuang KC, Wu Y, Giles W, Adamson J. Virtual patient-specific QA with DVH-based metrics. J Appl Clin Med Phys. 2022 Nov;23(11):e13639. doi: 10.1002/acm2.13639. Epub 2022 May 15. PMID: 35570395; PMCID: PMC9680566.
- Chuang KC, Giles W, Adamson J. A tool for patient-specific prediction of delivery discrepancies in machine parameters using trajectory log files. Med Phys. Mar 2021;48(3):978-990. doi:10.1002/mp.14670
Research Overview
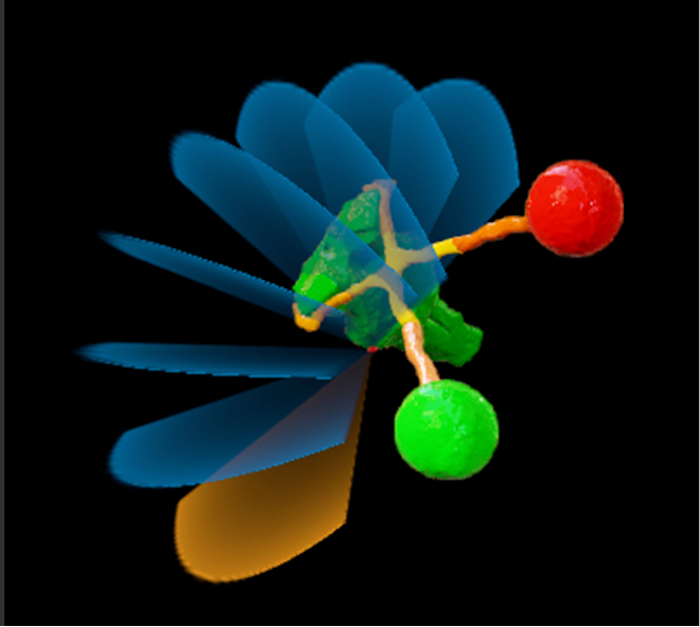
In the treatment planning of TGN using LINAC-based SRS, a single dose of 70-90 Gy is prescribed to the center of the TGN nerve at the root entry zone to the brainstem based upon MR images. Typically, 7-8 arc beams at different treatment table angles (i.e., non-coplanar beams in figure below) are arranged to ensure the maximum point dose is located within the trigeminal nerve while limiting the maximum dose of brainstem to < 32-36 Gy. A 4-mm cone applicator is used to target the radiation beam to a point within the trigeminal nerve. We have been investigating dosimetric impact due to the isocenter walkout for the LINAC-based SRS.
Investigators
Radiobiology, Theranostics and Radiomics
Research Overview
RECA (Radiation Enhanced by Cherenkov Photo-Activation) is a novel treatment approach (patented at Duke) that seeks to leverage Cherenkov light produced “naturally” by high-speed electrons in tissue during conventional radiation therapy. Cherenkov light is used to photo-activate photo-chemotherapeutic agents that create an additional anti-cancer therapeutic mechanism coincidental with the normal mechanisms of radiation therapy (ionization damage of DNA). A major high-value interest is that the novel RECA photo-damage component has the potential to initiate a systemic anti-cancer response (immune system mediated), which transforms radiation therapy from a local treatment to a systemic treatment, and could dramatically improve overall survival for many patients. This project is in collaboration with Tim Haystead, PhD, at Cancer Biology Lab, who has expertise in the design and creation of theranostic agents for RECA and other approaches.
Investigators
Research Overview
The discovery that famously inert noble gases like xenon exhibit, when inhaled, strong anesthetic properties was a surprise made even more puzzling by the further discovery that anesthetic potency varies with isotope. Xenon isotopes with zero nuclear spin exhibit the strongest anesthetic potency. This discovery has prompted speculation that quantum processes underpin some aspects of anesthesia. Further evidence has emerged from recent discoveries of long-lived quantum states in microtubules at room temperature, which has prompted further excitement that new discoveries into the physical foundations of anesthesia and consciousness may be possible involving quantum physics.
Investigators
Research Overview
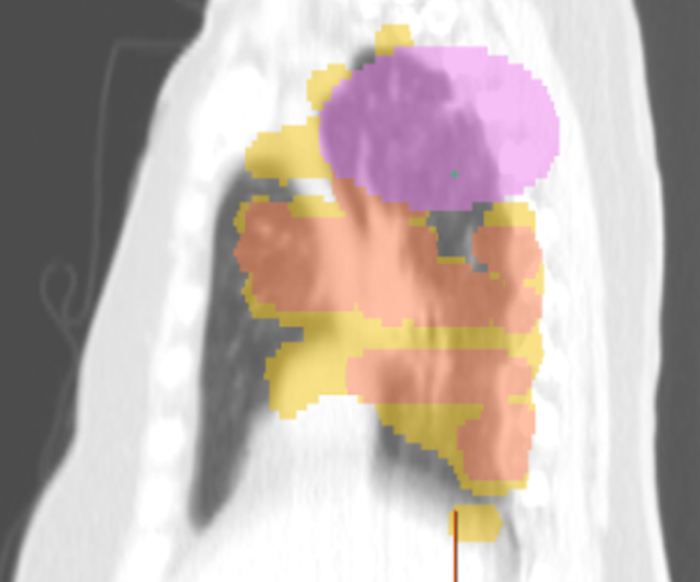
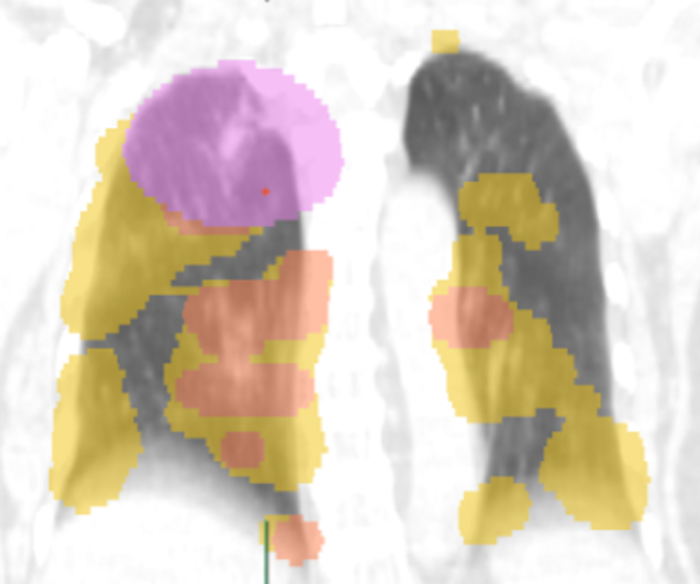
Stereotactic Body Radiation Therapy (SBRT) is a widely used, non-invasive treatment for early-stage non-small cell lung cancer (NSCLC), particularly in medically inoperable patients. While SBRT is generally well tolerated, a subset of patients – estimated at 6–12% – have underlying interstitial lung disease (ILD), a condition that significantly increases the risk of radiation-induced lung toxicity. Prior studies have shown that patients with ILD are at a markedly higher risk of developing radiation pneumonitis, with severe (grade ≥3) and even fatal (grade 5) toxicities occurring at much higher rates compared to patients without ILD. Despite these known clinical risks, the radiographic manifestations of SBRT-induced lung injury – especially the progression of fibrosis outside the irradiated field – remain poorly understood.
This retrospective study aims to deepen our understanding of SBRT-related toxicity in patients with ILD by analyzing radiographic and clinical data to evaluate whether SBRT triggers accelerated pulmonary fibrosis outside the irradiated area in patients with ILD. The study leverages advanced imaging analysis tools and computational modeling techniques to quantify lung changes and identify predictive imaging biomarkers. These analyses are designed to go beyond traditional clinical assessments and offer a more nuanced, data-driven understanding of radiation-induced lung injury. By integrating radiographic, clinical and computational data, this study seeks to provide a more comprehensive picture of SBRT toxicity in ILD patients. The findings could lead to improved risk stratification, personalized treatment planning and ultimately better outcomes for patients with lung cancer and coexisting ILD.


Investigators
Funding Sources
Duke Medical Physics Graduate Program Seed Funding
Automation and Emerging Treatment Technologies
Research Overview
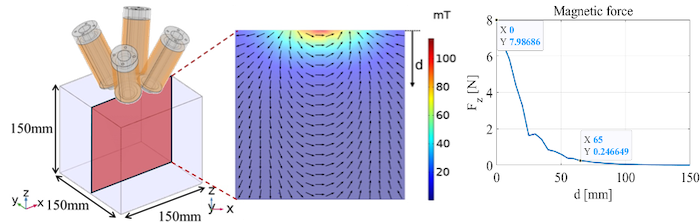
This collaborative research project explores the use of remote magnetic navigation systems to reduce gastrointestinal (GI) toxicity during stereotactic body radiotherapy (SBRT) for abdominal cancers, particularly when the bowel is in close proximity to the planning target volume (PTV). SBRT delivers high-dose radiation in a few fractions, which poses a risk of GI complications due to the radiosensitive nature of the bowel. Traditional methods struggle to safely displace bowel tissue away from the radiation field. The project leverages external electromagnetic arrays that manipulate magnetic objects inside the body. These systems have been used in various medical applications such as catheter guidance, capsule endoscopy and non-invasive surgery. Current research efforts include investigations into the dosimetric and logistical challenges with utilizing internal and external magnets during radiotherapy (COMSOL Multiphysics and TOPAS); applying endoscopic magnetic applying a remote magnetic navigation technology to demonstrate displacement of bowel in an ex vivo setting; and modeling the biomechanical properties of the abdomen so as to be able determine the required settings for the remote magnetic navigation system to achieve the desired bowel displacement from the PTV.




Investigators
Funding Sources
Duke Medical Physics Graduate Program Seed Funding
Research Overview
Our research focuses on quality control of radiotherapy data submitted for multi-institutional clinical trials, including image quality, contouring variability, delivery uncertainty, etc. A key component in conducting multi-institutional radiotherapy clinical trials is to reduce variability among different institutions and improve the robustness of research protocol design. This research aims to quantify uncertainties in the radiotherapy workflow, assess the impact of variability on treatment outcome and investigate and evaluate the strategies to improve the quality of radiotherapy clinical trial data.
Investigator
Selected Publications
- Cui Y, Yin F. Impact of Image Quality on Radiomics Applications. Physics in Medicine & Biology 2022; 67(15): 15TR03.
- Cui Y, Chen W, Kong FM, Olsen LA, Beatty RE, Maxim PG, Ritter T, Sohn JW, Higgins J, Galvin JM, Xiao Y. Contouring variations and the role of atlas in non-small-cell lung cancer radiotherapy: analysis of a multi-institutional pre-clinical trial planning study. Practical Radiation Oncology 2015; 5(2): e67-e75.
- Gondi V, Cui Y, Mehta MP, Manfredi D, Xiao Y, Galvin JM, Rowley H, Tome WA. Real-Time Pre-Treatment Review Limits Unacceptable Deviations on a Cooperative Group Radiotherapy Technique Trial: Quality Assurance Results of RTOG 0933. International Journal of Radiation Oncology * Biology * Physics 2015; 91(3): 564-570.
- Cui Y, Galvin JM, Parker W, Breen S, Yin F-F, Cai J, Papiez LS, Li A, Bednarz G, Chen W, Xiao Y. Implementation of Remote 3D IGRT QA for RTOG Clinical Trials. International Journal of Radiation Oncology * Biology * Physics 2013; 85(1): 271-277.
- Cui Y, Galvin JM, Straube WL, Bosch WR, Purdy JA, Li A, Xiao Y. Multi-System Verification of Registrations for IGRT in Clinical Trials. International Journal of Radiation Oncology * Biology * Physics 2011; 81(1): 305-312.


























