
by Sarah Brady

Ron Klarin’s cancer journey began in Florida with a CT scan that revealed a small lung nodule – one that his doctors initially dismissed as low-risk. “They told me it was probably nothing. There was no urgency,” he said.
At the time, Ron and his wife Bonnie were in the process of moving to North Carolina to be closer to family. After the move, his symptoms escalated, including severe coughing fits with any physical activity, prompting him to seek further care. A PET scan and biopsy at a hospital near his house revealed small cell lung cancer that had already spread to his bones and lymph nodes.
The initial rounds of chemotherapy were rough, leading to multiple hospitalizations. “After the first infusion, I was in the hospital for a week with sepsis. The second time, it was pneumonia and six days with chest tubes.” Looking for a better option and a more coordinated approach, Ron turned to Duke.

At Duke, Ron was introduced to Eugene Vaios, MD, MBA, a radiation oncologist and a member of the Duke Center for Brain and Spine Metastasis (DCBSM), after an MRI revealed two metastases in his brain. “That was a blow. I was devastated,” Ron said. “But meeting Dr. Vaios really changed my outlook. He put me so far at ease that I went from a state of high anxiety to, ‘Okay. Let’s go. Let’s do it.’”
Dr. Vaios recommended stereotactic radiosurgery (SRS), a focused, high-dose form of radiation that allows for targeted treatment that spares healthy tissue, provides local control and reduces side effects. “Dr. Vaios was extremely thorough,” said Ron. “We went through the scans multiple times and he explained everything in a way that made sense. That kind of attention builds trust. And I have to say, I love how he geeks out over what he does. I felt much more comfortable with SRS as opposed to whole-brain radiation,” which he feared would significantly impact his cognitive abilities.
SRS treatments made a measurable difference for Ron. “Anything that has not decreased is static, and the metastases in my brain have basically been eliminated,” said Ron. “There’s still some inflammation and necrosis, but it’s trending in the right direction.”
Ron continues to receive care at Duke and remains optimistic about his progress. “Small cell lung cancer isn’t easy to treat, but I’m very confident in the outcome of my treatment,” he said. “Just simply, Duke is fantastic. The care you experience, especially as a cancer patient – it really makes a difference where you go for your treatment, and I’ve been so impressed with the quality of care I’ve received here.”
Ron and Bonnie began donating to Duke in December 2024, and the couple recently became members of The Duke Tower Society – which honors those who have included Duke in their estate plans – when they committed a portion of their trust to the Duke Cancer Institute, with a focus on advancing cancer research. “I believe in the work being done here,” Ron said. “And we want to support it in a meaningful way.”

The DCBSM Model

Since its founding in 2017, the DCBSM has rapidly grown into one of the most comprehensive programs of its kind, treating patients whose cancer has spread to the brain, spine and other parts of the central nervous system. Duke Radiation Oncology is an integral part of the DCBSM team, delivering state-of-the-art SRS to patients with brain and spine metastases, as well as other complex neurological conditions. Led by Radiation Oncology Director John Kirkpatrick, MD, PhD, the team has a core group of central nervous system (CNS)–specific faculty, as well as various other faculty members who perform SRS.
“We’ve been doing radiosurgery at Duke as a collaboration between neurosurgery and radiation oncology in earnest since the early 2000s,” said Dr. Kirkpatrick. “But with the formation of the DCBSM, we’ve made the multidisciplinary secret sauce: adding palliative care and a strong medical oncology component to neurosurgery and radiation oncology.”

At the core of the Radiation Oncology Metastasis Team is a dedicated group of clinicians committed to treating the most challenging cases with precision and empathy. “I am so proud to be part of a simply outstanding multidisciplinary team that places top-level patient care first,” said Radiation Oncology Deputy Director for Research Scott Floyd, MD, PhD. “I know that the brain and spine mets patients that come to Duke receive the best care provided by a thoughtful and truly caring team.”
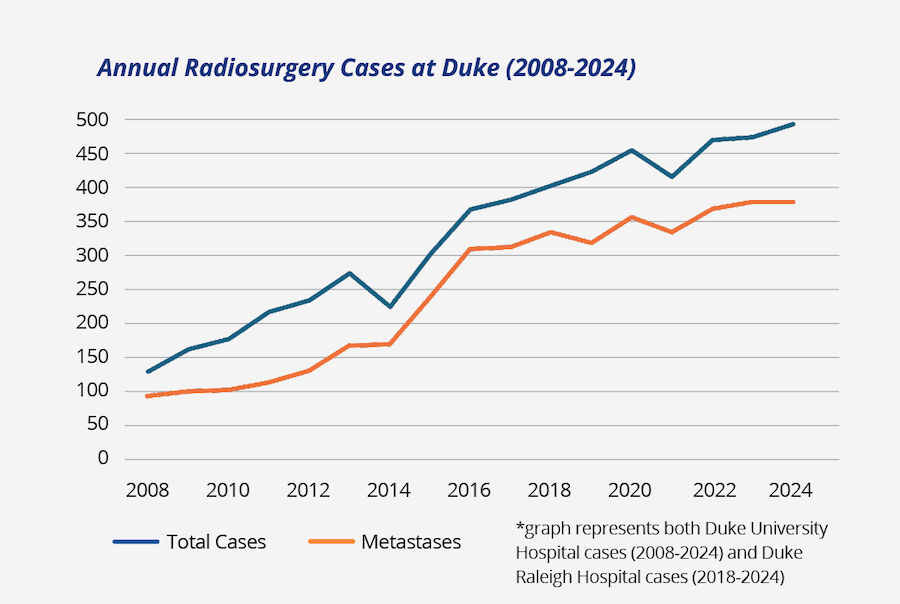
These providers routinely care for patients with multiple brain metastases – as well as other lesions like recurrent gliomas, acoustic neuromas, meningiomas and arteriovenous malformations – using SRS, “which has become a key weapon in the fight against brain, spine and base-of-skull disease,” said Dr. Kirkpatrick. “Over the past 20 years, we have treated over 5,000 patients with SRS and SBRT (stereotactic body radiation therapy).”
The program’s growth speaks for itself: in 2008, before the official founding of the DCBSM, Duke Radiation Oncology was treating just over 100 patients annually with SRS. By 2024, that number had surged to almost 500 patients annually, a 282% increase over a decade and a half.
A foundation of the program has been the outstanding leadership of and support by our radiation physics team. Medical physicists – including Justus Adamson, PhD; Yunfeng Cui, PhD; Joseph Kowalski, MS; Ke Lu, PhD; Julie Raffi, PhD; Anna Rodrigues, PhD; Chunhao Wang, PhD; and Yibo Xie, PhD – play a vital role in the radiation treatment of metastatic diseases. Physicists work alongside a multidisciplinary team throughout the entire patient care process, from treatment simulation, anatomy delineation and treatment planning to pre-treatment quality assurance and image-guided verification on treatment days.

“Our team is dedicated to delivering the highest quality care with efficiency and precision,” said physicist Chunhao Wang, PhD. “Beyond clinical service, our physicists also lead cutting-edge research, focusing on advanced imaging methods and artificial intelligence to improve radiation treatment consistency and better monitor disease outcomes. As a physicist, I feel privileged to be part of this wonderful team, and I truly believe our patients at Duke receive the best possible radiation care.”
This depth of experience – in both our physician and physicist teams – enables the team to tailor treatment strategies for individuals, optimizing outcomes and taking into account each patient’s goals of care.
The DCBSM Patient Care Difference

DCBSM’s model of care centers on rapid access and team-based navigation. Every patient referred to the Center is guaranteed an appointment within 72 hours. They are seen by a coordinated team of specialists – including radiation oncologists, neurosurgeons, medical oncologists and palliative care providers – on the same day and in one location. Each patient is matched with a navigator who helps streamline appointments and testing. “The treatment of patients with brain and spine metastases is often complex and requires input from multiple medical specialists,” said Radiation Oncology Deputy Director for Spine Metastases Trey Mullikin, MD. “Our Center excels at expediting multidisciplinary evaluations, enabling us to develop these patient-centered recommendations and ensuring that we deliver comprehensive treatment in a timely manner.”
Hope – and Results
Ultimately, what sets Duke Radiation Oncology and the DCBSM apart is the unwavering commitment to excellence, innovation and patient-centered care. “Our faculty and residents are leaders nationally and internationally, driving critical research forward and translating discoveries into tangible real-world solutions for patients every day,” said Dr. Vaios. “Because of the extraordinary people at Duke Radiation Oncology and the DCBSM, patients have access to best-in-class care, technology and clinical trials. This means better outcomes and a brighter future for patients at Duke and beyond.”
Palliative Care
In 2018, palliative care was integrated into the DCBSM as a half-day clinic in coordination with radiation oncology treatment, focused on supporting patients with serious illnesses and complex treatment plans. Since then, the service has expanded to five days a week, reflecting its increasing importance in enhancing patient care.

“The collaboration between palliative care and the DCBSM has been invaluable,” said Palliative Care Director Betsy Fricklas, PA-C, MMSc. “It allows us to offer a holistic approach that prioritizes not only disease treatment but also symptom management and emotional well-being.”
“Being part of the DCBSM has been a deeply meaningful and defining aspect of my career,” she continued. “It has allowed me to make a significant difference in the lives of patients and families, offering essential care during some of their most challenging times.”
Research, Innovation and Pushing Boundaries
“Looking forward, the really exciting part of the Center is that the research work we are doing will lead to even better results for our patients,” said Dr. Floyd. Over the past decade, the core CNS radiation oncology team has received nine federal grants, eight institutional grants, 13 foundation grants and three industry or private grants.
One significant project, led by Dr. Floyd, involves a multi-institutional consortium aimed at translating therapies for neurological diseases using organotypic brain slice cultures – which holds promise for developing new treatments for disorders like glioblastoma. Another initiative is the NIH-funded K08 study led by Dr. Reitman on enhancing the efficacy of radiation therapy for pediatric brainstem gliomas by targeting ATM. Beyond federal funding, the team has entered into partnerships, like the recent collaboration with Caris Life Sciences, in which Drs. Vaios, Floyd and Reitman are investigating the potential of circulating tumor DNA as a non-invasive biomarker for glioblastoma. All of these efforts reflect the team’s ongoing commitment to improving patient care through research and technology. “The support from federal, foundational and philanthropic funding sources is critical to our mission of improving patient care for patients with brain and spine tumors,” said Zach Reitman, MD, PhD.
New Research Insights
Major published findings in the last two years include the largest single-institution series to report outcomes with SRS and immunotherapy – and the first to evaluate long-term outcomes with dual immune-checkpoint inhibition (ICPI) – which found that offering dual ICPI to patients with melanoma or non-small cell lung cancer who are receiving SRS for brain metastases significantly improves local and distant intracranial control (International Journal of Radiation Oncology, Biology, Physics, 2024).

In addition, in 2025, the team found that the timing of radiosurgery and dual immune-checkpoint blockade matters. While combined modality therapy improved cancer control, patients receiving dual immune-checkpoint blockade within four weeks of radiosurgery had higher risk for symptomatic radiation necrosis, or injury and inflammation to normal brain tissue. These results from a cohort of 288 melanoma and lung cancer patients at Duke (JAMA Network Open, 2025) provide critical guidance for physicians to optimize the timing and sequencing of novel therapies to maximize cancer control while reducing risks for patients. Read more high-impact research at duke.is/DCBSMstudies.
Clinical Trials
Brain and spine metastases have often historically excluded patients from clinical trials. At the DCBSM, clinical trials are designed specifically for patients with metastases, and especially focused on personalized approaches.
From imaging techniques like quantitative magnetic resonance imaging to assess spinal metastases after SBRT (Dr. Mullikin); to exploring the diagnostic accuracy of delayed MRI contrast enhancement for radiation necrosis in brain metastases (Dr. Floyd); to trialing parenteral ascorbate-meglumine as a novel magnetic resonance imaging-guide adjunctive therapeutic for SRS (Dr. Kirkpatrick), the clinical trials offered at the DCBSM highlight Duke’s leadership in precision medicine and commitment to our patients.